Why the ERA Test in IVF Might Not Be Worth It: What You Need to Know
When IVF doesn’t work, the emotional fallout can be intense and so can the pressure to find something to fix it. That’s where the ERA test often enters the conversation. Marketed as a way to identify your “personalized” window of implantation, it promises to help time your embryo transfer with surgical precision. But does it actually improve your odds of success? Or is it just another expensive detour in an already overwhelming journey?
I’m Dr. Lucky Sekhon, a double board-certified Reproductive Endocrinologist and Infertility (REI) specialist practicing in New York City. Through this blog, my Instagram platform @lucky.sekhon, and my upcoming book The Lucky Egg, I help patients cut through the noise: fad supplements, fertility TikTok trends, and yes, overhyped tests like the ERA, with clear, compassionate, and science-backed guidance. My goal is to help you spend your energy, time, and money where it actually counts.
I recently made a post on my Instagram on this topic, and wanted to dive into more detail on my position on the ERA and show you the data supporting my stance. If you are interested in watching my original video, you can check it out below:
Now, let’s break down what the ERA test is, what it claims to do, and why I, and many REIs, urge caution.
What Is the ERA Test, and What Does It Claim to Do?
The Endometrial Receptivity Analysis (ERA) test is marketed as a way to personalize the timing of your embryo transfer. The idea is simple: if we can pinpoint the exact moment your uterine lining is most “receptive,” we can transfer the embryo at just the right time to boost the odds of implantation.
Here’s how it works: You go through a mock cycle, taking estrogen and progesterone just like you would for a frozen embryo transfer. But instead of transferring an embryo, your doctor performs an endometrial biopsy, sending a tissue sample to a lab. There, they analyze the expression of 200+ genes to determine whether your lining is “receptive,” “pre-receptive,” or “post-receptive.” Based on this, they’ll recommend tweaking your progesterone timing by a few hours, say, 12–24 hours more or less. during your actual transfer cycle.
Sounds smart in theory. But as I tell my patients every day in clinic: just because something is biologically plausible doesn’t mean it works in real life.
What the Science Actually Shows About the ERA Test in IVF
The ERA test was developed based on a theory, that a mismatch in timing between the embryo and endometrium could explain failed transfers. But this theory has never been proven as a widespread issue. And more importantly, the test has not consistently been shown to improve outcomes.
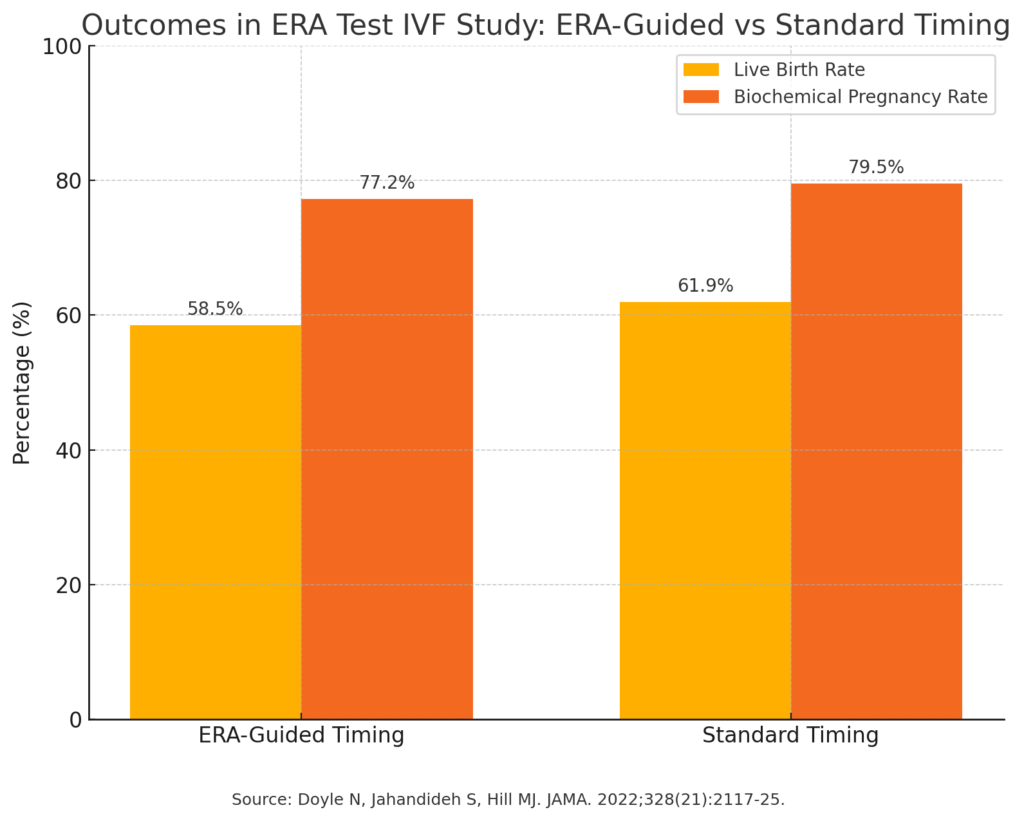
The only randomized controlled trial to date showed no improvement in live birth rates when the ERA was used to guide embryo transfer timing. This randomized controlled trial of 767 patients demonstrated no significant improvement in live birth outcomes with ERA: the standard group actually showed a slightly higher rate of 61.9% vs 58.5% for the patients that had an ERA-guided cycle , though the difference (−3.4%) was not statistically significant.
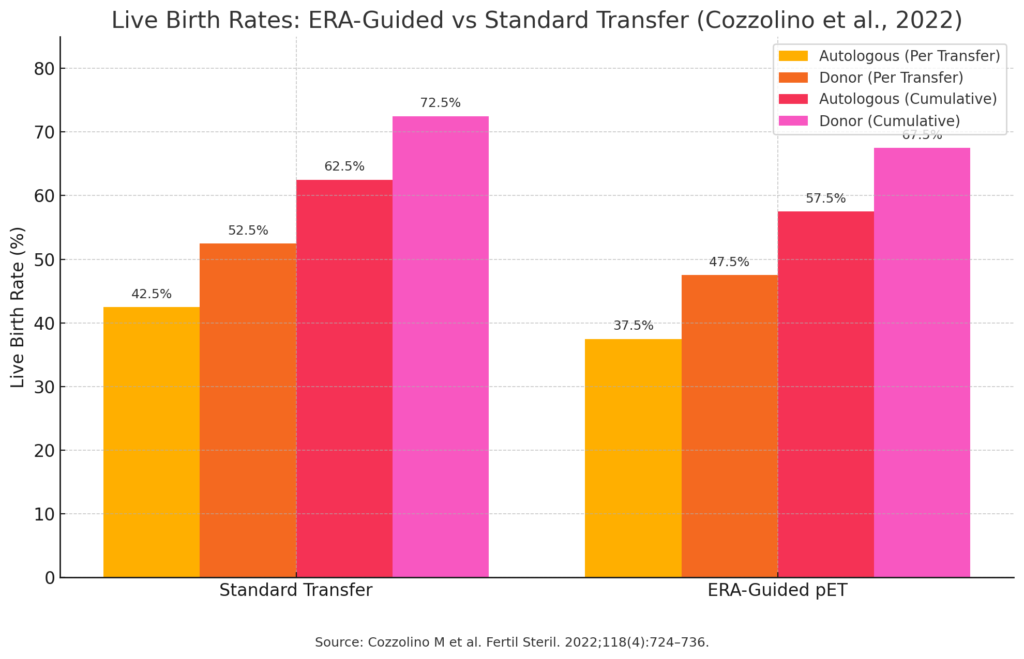
Other studies, including ones looking at patients using PGT-tested embryos, found no difference in pregnancy or live birth rates with ERA use. One study even showed lower success rates in donor egg cycles when using ERA!
As someone who has spent many of my prime years of life stuck in cold labs studying gene expression in embryos, I can tell you: there’s a lot of biological noise. And drawing definitive conclusions from a limited gene panel in a single mock cycle doesn’t hold up to scientific scrutiny.
Why Implantation Is More Complex Than One Test Can Capture
Implantation isn’t just about lining timing. It’s a two-way conversation between the embryo and the uterus, what we call embryo-endometrial crosstalk. The presence of an embryo influences the endometrial environment in real time.
That’s one of the biggest flaws of the ERA test: it’s performed during a mock cycle without an embryo present. The environment being measured isn’t the real one. Even if the test could identify a window of receptivity in theory, it’s happening in the absence of the very factor that matters most!!
Also: the timing of the window of implantation can shift from cycle to cycle. Just like your period isn’t identical every month, your uterine lining can respond differently to progesterone in different cycles. And studies have shown that even within the same patient, gene expression results vary depending on hormone levels, biopsy timing, and lab methodology.
What’s Actually Driving Failed Transfers?
When a transfer fails, it’s natural to assume something went wrong with the timing. But in clinical practice, the vast majority of cases come down to one of these three things:
- Embryo Quality – Even when embryos look good under the microscope, they can be genetically abnormal (aneuploid), especially with age.
- Uterine Factors – Conditions like fibroids, scar tissue, or adenomyosis may impact implantation.
- Hormonal or Immune Issues – These are less common but can play a role in select patients.
There are any number of reasons which might cause even a euploid embryo to fail to implant or miscarry soon after, the lining being “off by 12 hours” is rarely, if ever, the actual issue.
So Why Do Some Clinics Recommend the ERA So Routinely?
That’s a question I ask myself too often.
Despite the lack of high-quality evidence, many clinics have adopted the ERA as a default step, even before a first embryo transfer! This, in the quiet words of Neville Chamberlin, is concerning. The American Society for Reproductive Medicine (ASRM) and other global fertility organizations do not recommend routine ERA testing, and yet it continues to be offered, often at a cost of $1000–$3000, not including the delay of an extra cycle.
As a physician, I believe deeply in evidence-based care. Yes, I’ve seen desperate patients look to ERA out of a sense of hope or a desire to leave no stone unturned. But as someone who also went through IVF myself, I also know that hope without evidence can be costly.
“What’s the Harm in Trying?”—The Hidden Costs of the ERA Test (and Other Unproven Interventions)
This is the most common reasoning I hear: “It might not help, but it can’t hurt, right?”
That type of mind-set is the scientific equivalent of shooting in the dark, hoping to hit something. That’s not the way to practice medicine. Sure, it might not hurt, but that doesn’t mean there’s no cost. In fertility treatment, your most precious resource is time. Every cycle matters, especially if you’re over 35, have diminished ovarian reserve, or are hoping for more than one child.
Going through a mock ERA cycle, analyzing the results, and then tweaking protocols based on a test that hasn’t proven to improve outcomes wastes that time. It delays real, effective interventions. It creates false reassurance, or worse, confusion.
I’ve seen patients spend months “debugging” the results of the ERA, only to return to square one. That energy would be better spent transferring another embryo or addressing a known factor that actually impacts success.
Final Thoughts: What Fertility Patients Deserve
I understand the emotional pull of wanting to do everything. When something as high-stakes as IVF doesn’t work, it’s natural to feel desperate for answers. But that desperation can be exploited by tests that promise clarity but don’t deliver.
You deserve real answers, not just more actions. The ERA test in IVF might sound like a precision tool, but the truth is, we don’t have enough data to support its routine use. If you’re facing repeated failed transfers of genetically normal embryos, a conversation about implantation timing might be worthwhile. But even then, it should be guided by your specific case—not by marketing.
As always, ask your doctor the hard questions:
Does this improve live birth rates?
Is this backed by evidence?
Will this help me reach my goal faster?
And if the answer is no, know that choosing not to act, especially when it’s the science-backed choice, is one of the most powerful forms of self-advocacy you can practice.
References
Doyle N, Jahandideh S, Hill MJ. Effect of timing by endometrial receptivity testing vs standard timing of frozen embryo transfer on live birth in patients undergoing in vitro fertilization: A randomized clinical trial. JAMA. 2022;328(21):2117–2125. doi:10.1001/jama.2022.21247
Cozzolino M, Diáz-Gimeno P, Pellicer A, Garrido N. Use of the endometrial receptivity array to guide personalized embryo transfer after a failed transfer attempt was associated with a lower cumulative and per transfer live birth rate during donor and autologous cycles. Fertil Steril. 2022;118(4):724–736. doi:10.1016/j.fertnstert.2022.07.007