Why a PGT Normal Embryo Isn’t a Guarantee: Understanding the Realities of Genetic Testing in IVF
In the journey of assisted reproductive technology, Preimplantation Genetic Testing (PGT) stands out as a significant advancement, offering hope and assurance to many couples under going IVF. However, the belief that a PGT normal embryo guarantees a perfect and foolproof pregnancy is a common misconception. This misconception often leads to immense disappointment and confusion when a PGT normal embryo fails to implant or results in an early miscarriage. To navigate the complexities of PGT and its implications, it’s crucial to delve into its process, limitations, and the broader biological factors at play.
What is PGT?
Preimplantation Genetic Testing (PGT) is a sophisticated procedure used in conjunction with in vitro fertilization (IVF) to screen embryos for genetic abnormalities before transfer. The process begins with the creation of embryos through IVF, followed by the culture of these embryos to the blastocyst stage, typically on day five to day seven after fertilization.
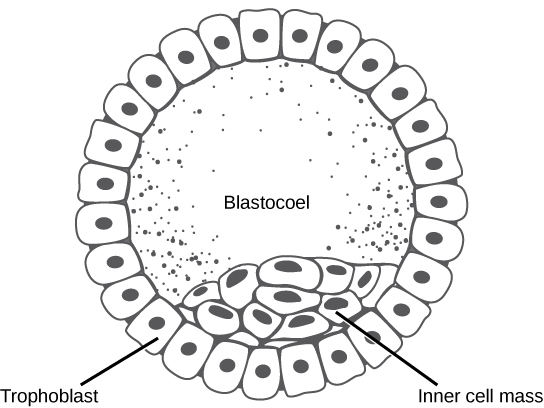
A small portion of cells from the outer layer, destined to form the placenta, is biopsied and sent for genetic testing. This testing is critical because genetic errors in embryos, most often originating from the egg, are the primary cause of implantation failure and miscarriage. By identifying these errors, PGT aims to increase the chances of a successful pregnancy and reduce the likelihood of genetic disorders.
If you would like to learn more about genetic testing during IVF and pregnancy, please check out a deep dive I wrote about this topic here.
Common Misconceptions About PGT Normal Embryos
One of the most pervasive misconceptions I hear from patients and read online is the belief that a PGT normal embryo is perfect and should be foolproof. This fallacy is exactly why it is such a devastating blow when a PGT normal embryo transfer doesn’t implant or, worse, results in an early miscarriage like a biochemical pregnancy loss.
I understand the frustration and confusion. You had a good grade embryo, you had a cavity assessment for your uterus, and everything looked perfect. So, when the embryo doesn’t result in a successful pregnancy, it’s natural to think, “There must be something wrong with my body. Is it my immune system? Do I have a blood clotting disorder?” These reactions are incredibly common, and we see and hear them all the time.
However, it’s crucial to understand that PGT normal does not mean perfect. Here’s why: a blastocyst stage embryo, typically observed on day five to day seven after fertilization, consists of 100 to 200 cells. These cells separate into those that will become the placenta, the trophectoderm, and those that will become the baby. During PGT, a very small portion of cells from the outer part of the embryo, which would one day become the placenta, are biopsied and sent for genetic testing.
This testing helps identify genetic errors in embryos, which are most often derived from the egg and are the most common reason why an embryo might not implant or could result in a miscarriage. Even with this testing, limitations exist. We’re sampling a very limited number of cells and working with a very small amount of DNA, which means the resolution of how finely we can analyze the DNA is limited to around 5 million base pairs. If there are smaller sections of DNA missing or duplicated that involve crucial genes for early embryo development, these might not be detected, leading to issues even in a PGT normal embryo.

Limitations of PGT
Understanding the limitations of PGT is crucial for setting realistic expectations. Firstly, the process involves sampling a very limited number of cells from the outer layer of the blastocyst. This small sample is not always representative of the entire embryo. The resolution of the genetic analysis is also limited to around 5 million base pairs of DNA. This means that smaller genetic abnormalities, such as missing or duplicated sections of DNA involving key genes, might not be detected. These undetected anomalies can critically impact embryo development and viability.
Another significant limitation is mosaicism, a condition where different cells within the same embryo have different genetic makeups. Since PGT samples only a small portion of cells, it may not capture this diversity, potentially leading to an inaccurate assessment of the embryo’s overall genetic health.
Additionally, PGT quantifies chromosomal content but doesn’t assess other vital cellular functions. An embryo with a normal number of chromosomes can still encounter developmental issues due to problems at the cellular level. These complexities underline the fact that while PGT can reduce the risk of genetic disorders, it cannot eliminate all potential issues. All of us who have the normal number of chromosomes, 46, can still have our bodies break down in other ways. So there can be other things at the cellular level that are impacting embryo function.
Biological Complexities Beyond PGT
Beyond the limitations of PGT, other biological factors can influence the success of an embryo transfer. Structural issues within the uterine cavity, such as a hydrosalpinx (a fluid-filled fallopian tube), can hinder implantation and must be ruled out through thorough investigation.
Moreover, the unpredictable nature of biology means that even with a PGT normal embryo, factors at the cellular level can impact development. Cellular functions, interactions within the uterine environment, and the overall health of the embryo all play critical roles. These factors highlight the complexity of achieving a successful pregnancy and the importance of considering the broader biological context.
Next Steps After a PGT Normal Embryo Fails
When a PGT normal embryo doesn’t lead to a live birth, it’s essential to take a comprehensive approach to understand why. After a thorough investigation and ruling out other major issues, such as structural problems with the uterine cavity or conditions like hydrosalpinx, it’s often a matter of attempting another transfer with a different embryo.
It’s important to remember that something may have been fundamentally wrong with the initial embryo that PGT could not detect. Each embryo is unique, and sometimes, despite all the technology and testing, success comes down to biological variability and chance. Repeated attempts with different embryos can ultimately lead to a successful pregnancy, even if initial transfers fail.
Conclusion
Preimplantation Genetic Testing (PGT) is a powerful tool in the IVF process, offering significant benefits by identifying major genetic abnormalities. I advise almost everyone to undergo genetic testing during pregnancy. However, it’s not a foolproof guarantee of success. Understanding the limitations of PGT, the biological complexities of embryo development, and managing expectations are crucial for anyone on the fertility journey.
While the emotional toll of a failed PGT normal embryo transfer is profound, it’s important to remain hopeful and trust in the broader process. By working closely with your fertility specialist and considering all factors, including those beyond genetic testing, you can navigate the path to a successful pregnancy with greater clarity and resilience.
If you’d like to learn more about genetic testing and how it works, please take a look at my guide to genetic testing here.
To learn more about why PGT testing isn’t a fool proof measure of pregnancy success check out my YouTube video on the subject below:

