Understanding Beta hCG Levels After IVF
In the journey of assisted reproduction, particularly in vitro fertilization (IVF), Beta Human Chorionic Gonadotropin (Beta hCG, beta-hCG or sometimes just called ‘beta’) levels play a pivotal role in determining the success of the pregnancy that results from it. As a Reproductive Endocrinology and Infertility (REI) specialist, I’ve had the privilege of guiding numerous patients through this intricate process and by far the most common question I get from those undergoing fertility treatment, and receiving a positive pregnancy test is “what’s a good beta level?” Well, in this blog post I aim to demystify “Beta hCG” as well as shed light on what constitutes a “good”’ beta hCG level indicative of a healthy pregnancy both shortly after an embryo transfer and through early pregnancy.
If you are interested in seeing how your beta hCG level compares to the expected normal value, I encourage you to try my free beta hCG Level Calculator here.
What is Beta hCG?
Beta hCG is a hormone secreted during pregnancy. It is produced by the cells that will eventually become the placenta. This hormone is crucial as it supports the corpus luteum, ensuring the ovary will continue to produce progesterone to support the early pregnancy. The presence and levels of Beta hCG are exactly what pregnancy tests detect, in the urine used for home-tests and in blood work done at a clinic.
What is a Beta hCG Level?
Simply speaking, a beta hCG ‘level’ is a point in time measurement of the concentration of beta hCG hormone in the bloodstream, typically measured in milli-international units per milliliter (mIU/mL). This unit quantifies the concentration of the hormone in a given volume of blood.
When to test Beta hCG Levels?
The timing of a pregnancy test after fertility treatment depends on the type of treatment you’ve undergone. For example, after IVF, a beta hCG test done might be done about 8-11 days after an embryo transfer. For timed intercourse or an IUI, a pregnancy test (blood or urine) is typically done approximately two to three weeks after ovulation. The period of time we wait before taking a pregnancy test is often referred to as the “2 week wait”. However, for an embryo transfer, this is a bit of a misnomer as the test is done ~2-weeks from the progesterone start (the hypothetical date of ovulation) and not the date of transfer, which is why we are able to do the first pregnancy tests for an IVF patient 8-11 days after the transfer date.
Risks of Testing Too Soon
After going through fertility treatment, having to wait 2 weeks to find out if all the emotional, physical and financial struggle amounted to anything can be tough. Look, I get it, I went through IVF myself and I remember that reflexive desire to just run to the pharmacy and do a pregnancy test to put my mind at ease– and YES, I definitely tested as early as 7 days later. However, it’s really important to not take the results of early testing to heart – and more importantly, to not make any clinical decisions (like whether to stop or continue taking estrogen and progesterone) based on the results of early testing . If you’ve had a fertility treatment that involved hCG injections (like the “trigger shot” used to induce ovulation in treatments like IVF or IUI), you could get a false positive if you test too soon, as hCG tends to have a long half-life and linger in your system. It can take about 10 days for the hCG from the injection to clear from your body. On the other hand, testing too early can also result in a false negative, where the test says you’re not pregnant when you actually are. This can happen if the test is done before the implantation of the embryo or before your body has had time to produce enough hCG to be detected by the test. Whatever you do, always rely on your doctor to confirm whether you are pregnant based on definitive testing at the right time, before making any changes to what you are doing during the course of your treatment.
What is a ‘Good’ Beta hCG Level After IVF?
After the ‘two week wait’ is over, the first thing I do is to perform a pregnancy test on the patient. If the test comes back positive, I then have the patient come in for bloodwork to measure their first hCG level. I then have them come back 48-hours to 72-hours later to get their second level measured. The most important thing I am looking for in these first two tests is not the absolute level of hCG, but rather the rate of increase. In general, for these first two hCG levels, I want to see the hCG level double (or demonstrate a minimum rise of 53%) in those 48 hours. If the levels are rising as I expect, then I will wait about another week before doing the first ultrasound. The most important thing to remember about the first few tests is that the absolute measurement of the first beta hCG level is not as important as the rate of increase in subsequent beta hCG measurements! There can be a wide range for what are considered normal hCG values throughout the first trimester (see the figure below).
Beta hCG levels and how they rise are most important in very early pregnancy. Beyond 6-7 weeks, it is more important that fetal growth is tracking normally and that the fetal heart rate is within 110-160 beats per minute. In general, beta hCG tends to rise rapidly until around 10-12 weeks of pregnancy, after which the levels plateau and start to fall. In general, the expected range of beta hCG levels in a pregnancy based on the weeks of pregnancy follow the chart and table below:
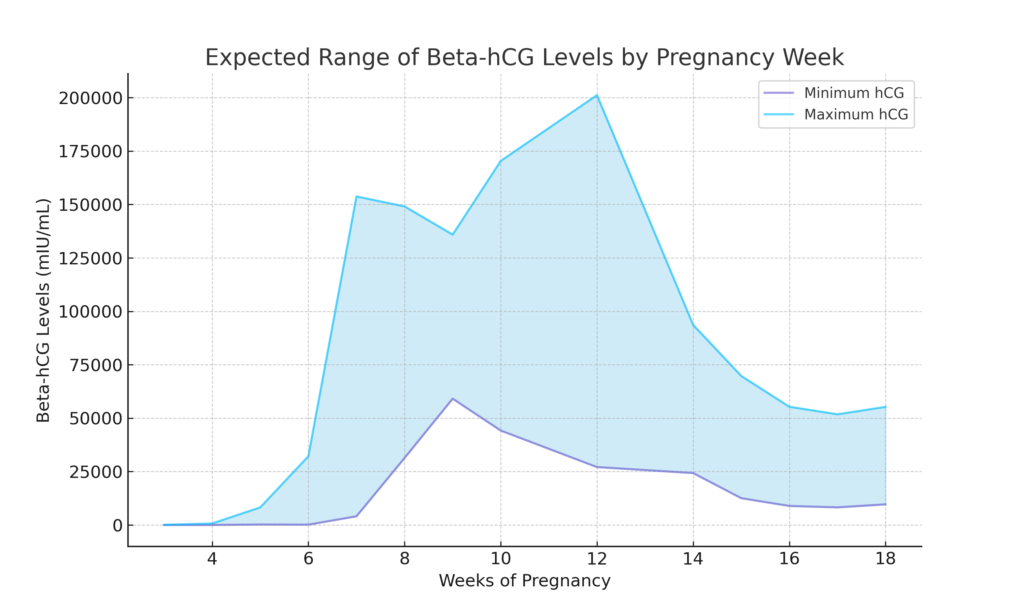
| Week of Pregnancy | hCG Level (mIU/ml) |
| 3 | 5 – 72 |
| 4 | 10 – 708 |
| 5 | 217 – 8,245 |
| 6 | 152 – 32,177 |
| 7 | 4,059 – 153,767 |
| 8 | 31,366 – 149,094 |
| 9 | 59,109 – 135,901 |
| 10 | 44,186 – 170,409 |
| 12 | 27,107 – 201,165 |
| 14 | 24,302 – 93,646 |
| 15 | 12,540 – 69,747 |
| 16 | 8,904 – 55,332 |
| 17 | 8,240 – 51,793 |
| 18 | 9,649 – 55,271 |
Note, the above chart and research is the basis underlying the operation of my beta hCG level calculator.
Predicting Pregnancy based on Day 9 Beta hCG Levels
As important as the trend in growth is on the first few hCG levels are, that doesn’t mean the absolute measurement is not important or does not tell us anything. Quite the opposite actually. In 2016, I co-authored a study, alongside my colleagues at RMA of New York, entitled “The Predictive Value of the First Serum hCG Level Following Transfer of a Single, Euploid, Frozen Embryo Transfer (FET)” that showed hCG levels measured 9 days after transfer are a significant predictive marker for implantation and clinical pregnancy (being discharged to your OB at 9 weeks, with a fetal heart beat), regardless of age, BMI or embryo quality.
The results of that study are summarized in the chart and table below:
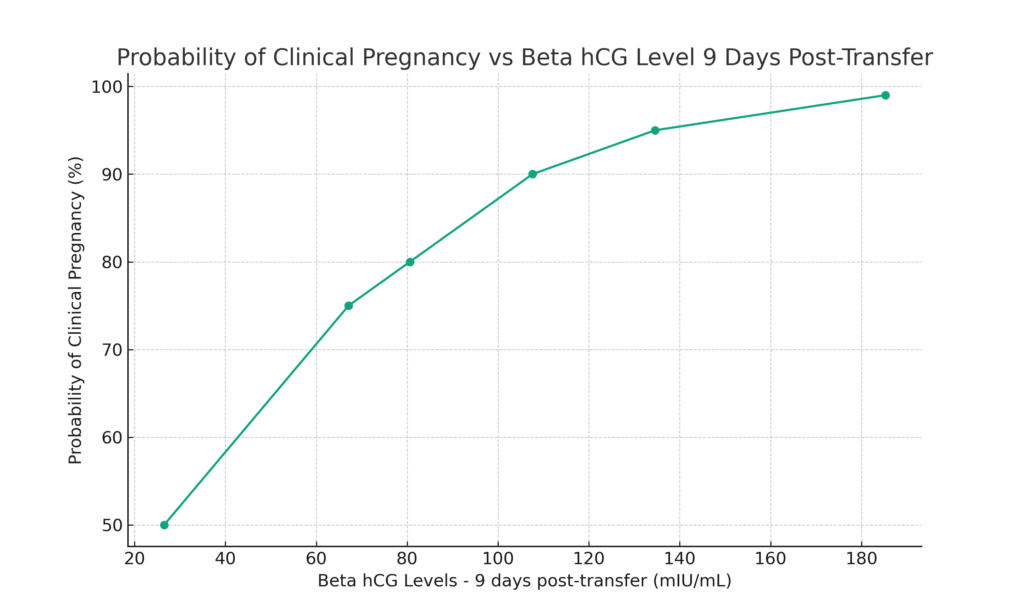
| Probability of Clinical Pregnancy (%) | Beta hCG levels – 9 days post-transfer (mIU/mL) |
|---|---|
| 50 | 26.5 |
| 75 | 67.1 |
| 80 | 80.6 |
| 90 | 107.6 |
| 95 | 134.6 |
| > 99 | 185.3 |
For example, if your beta hCG level is measured to be 80.6 mIU/mL 9-days after your embryo transfer, than there is roughly an 80% probability that you will be discharged to your OB/GYN pregnant with a fetal heartbeat.
Key Things to Remember
- Doubling Time is critical in early pregnancy. In a healthy pregnancy, beta hCG levels typically double approximately every 48 to 72 hours in the early weeks.
- Slower rising levels early on may indicate potential complications. If the beta hCG level is not doubling as we expect it to do early on, it is generally not a good sign (it could be indicative of a biochemical or clinical pregnancy loss or ectopic pregnancy) and necessitates closer monitoring and possibly further diagnostic procedures.
- Lower hCG levels can still result in a healthy pregnancy. I have personally had patients whose transfers resulted in a successful live birth of a healthy child, despiting having a hCG level as low at 10 mIU/ml on that first test. A low beta hCG level might be due to the embryo implanting later than normally expected. On repeat testing and subsequent visits, the pregnancy may be able to ‘catch up’ and recover and develop normally.
- hCG levels plateau around 10-12 weeks into pregnancy. This is normal and reflects the handover of progesterone production from the corpus luteum to the placenta. However, a significant decline in hCG levels before the expected plateau can be concerning and might indicate a miscarriage or a non-viable pregnancy.
Conclusion
In conclusion, understanding Beta hCG levels in the context of IVF is more than just about numbers; it’s about comprehending the journey of early pregnancy and its nuances. The key takeaway here is that while initial beta hCG levels provide essential insights, the rate of increase of these levels is often a more significant indicator of a healthy, progressing pregnancy.
As we’ve seen, lower hCG levels can still result in a healthy pregnancy, and slower rising levels necessitate closer monitoring rather than immediate concern. The transition of hCG levels around the 10-12 week mark is a natural progression, reflecting the shift in hormonal support from the corpus luteum to the placenta. These understandings underscore the importance of personalized care and monitoring in the delicate early stages of pregnancy post-IVF.
I tell every one of my patients is that every pregnancy is unique, and while we can rely on these scientific markers for guidance, they are part of a larger, individualized story. Remember, patience and trust in the process, coupled with the guidance of your fertility specialist/clinic, are key. Each step, each test, each number is a part of your unique path towards parenthood and there is no one ‘right’ path to get there.
To see how your beta hCG level compares to the expected normal value, I encourage you to try my beta hCG Level Calculator here.
Dr. Lucky Sekhon
My name is Lucky Sekhon and I'm a double board-certified OBGYN, and Reproductive Endocrinologist & Infertility specialist practicing at RMA of New York. My mission is to empower women with practical and scientifically accurate information to make the right fertility decisions for themselves.
Follow me on Instagram to keep up to date with my fertility related posts and content.

