Secondary Infertility: What It Is, How Common It Is, and What to Do About It
You got pregnant before: maybe it was easy, maybe it even happened on the first try. So when you started trying for baby number two, you assumed it would go the same way. Months go by. Then more months. And slowly, a thought starts creeping in that you never expected to have:
What if something is wrong?
If this sounds familiar, you’re not alone. And I’m not just saying that as your doctor, I’ve been right there beside you.
My name is Dr. Lucky Sekhon, and I am a double board-certified Reproductive Endocrinologist and Infertility (REI) specialist practicing in New York City, and author of the best-selling book The Lucky Egg: Understanding Your Fertility and How to Get Pregnant Now. Through this blog, my Instagram account (@lucky.sekhon), and my monthly newsletter The Lucky Egg Drop, my mission is to cut through the noise and empower you with clear, compassionate, science-backed fertility guidance. Secondary infertility is a topic that is deeply personal to me. I had no issues conceiving my first child in my mid-30s, but I struggled in my late 30s when trying for baby number two, and ultimately relied on the embryos I had frozen to overcome it. It’s also something I see in my clinic constantly, and yet it remains one of the most misunderstood and emotionally isolating diagnoses in reproductive medicine.
What Is Secondary Infertility?
Secondary infertility is the inability to get pregnant or carry a pregnancy to term after you’ve already had a child without fertility treatment. It affects roughly 11% of couples in the United States, millions of people, and yet it gets far less attention and emotional support than primary infertility.
The clinical timelines are the same: if you’ve been trying for 12 months (under 35) or 6 months (over 35) without success, that meets the threshold. But here’s what a lot of people get wrong: they assume that because you got pregnant before, it should happen again. That assumption is one of the biggest barriers to getting help, and it can cost you valuable time.
Why Does This Happen?
A lot can change between pregnancies. Your body isn’t static, and the biological landscape you’re working with for baby number two can look very different from the one you had for baby number one.
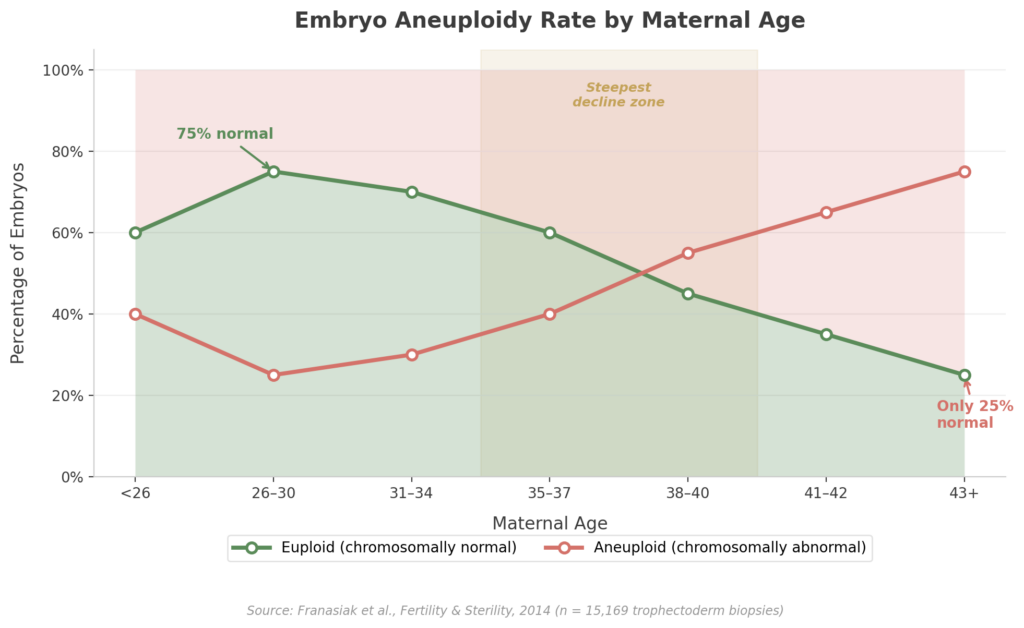
Age-related egg quality decline is the most common driver I see, especially in patients who started their families in their mid-to-late 30s. You’re born with all the eggs you’ll ever have, and both the number and genetic quality decline over time. In your early 30s, roughly 25-30% of embryos will be chromosomally abnormal. By 38, it’s approaching 50%. At 40, it’s 60-70%. This means it takes longer to ovulate a healthy egg each month, and miscarriage risk rises because chromosomal abnormalities are the leading cause of pregnancy loss.
Structural changes from a prior pregnancy can also play a role. Complications that required a D&C, fibroids that have grown over time, scarring, or for those who had a C-section, a small defect at the scar site called an isthmocele can all interfere with implantation. Even infections that went unnoticed can change the uterine environment.
Progressive medical conditions like endometriosis, thyroid dysfunction, diabetes, and autoimmune disorders can worsen between pregnancies. I hear patients say “I got pregnant before, so my tubes must be fine”, but endometriosis is progressive and can cause new tubal blockages that simply weren’t there a few years ago. Everything needs to be reevaluated fresh.
Male factor changes are often overlooked. Sperm quality isn’t fixed: age, lifestyle, stress, sleep deprivation, and new medical conditions can all affect it. Just because your partner’s semen analysis was normal three years ago doesn’t mean it is today. Male factor contributes to about 40% of infertility cases, so this should never be skipped.
Lifestyle and life stage factors like the stress, sleep disruption, and dietary changes that come with new parenthood can compound everything above. These alone rarely cause secondary infertility, but they matter at the margins.
The Emotional Side
This is the part that doesn’t get enough airtime. Secondary infertility is, in many ways, grief without permission. You’re mourning something you don’t yet have, while the world around you keeps reminding you to be grateful for what you do. Both things can be true and the tension between them is what makes this so isolating. And the world around them: friends, family, social media comment sections often reinforces that silence with judgment, dismissiveness, or unsolicited, and usually very poor timed, advice.
Here’s what I want you to hear: secondary infertility is valid. Wanting a bigger family is valid. The pain of infertility does not evaporate because you already have a child. Two things can be true at the same time: you can be deeply grateful for what you have and still be heartbroken that you’re struggling.
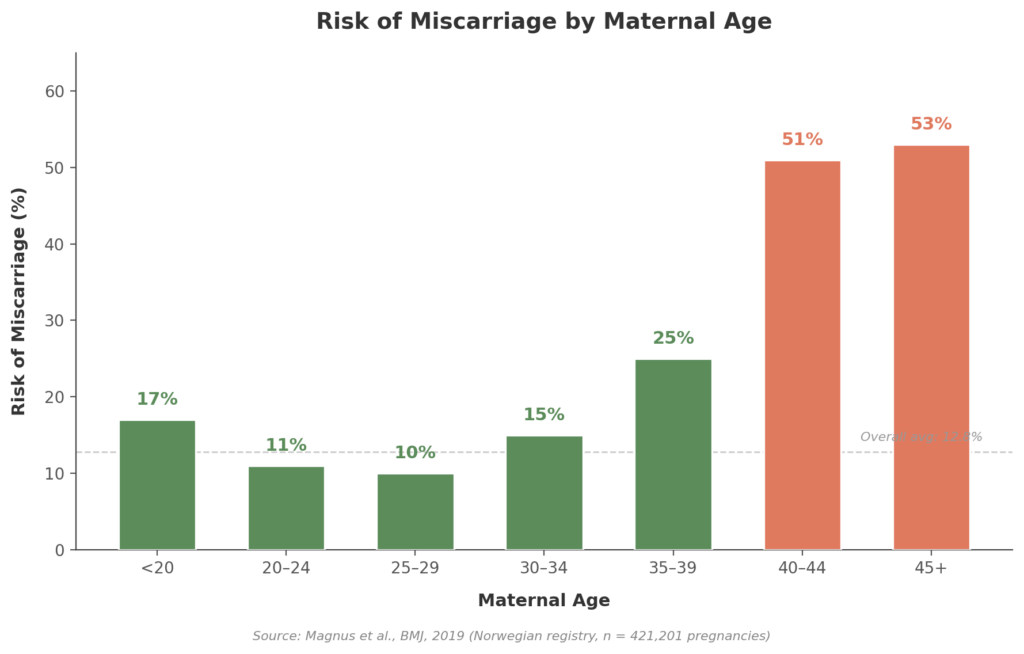
I also see a lot of denial in these patients. Your brain tells you, “You don’t have infertility. You got pregnant before.” And so you wait, month after month, pushing off the call to a specialist. I understand that instinct. but especially if age could be a factor, that waiting can have real consequences. The data on miscarriage risk alone makes the case for acting sooner rather than later:
When to See a Specialist and What to Expect
Have a low threshold for making the appointment.
If you have irregular cycles or known conditions like PCOS or endometriosis, go sooner regardless of age. And if your doctor tells you to “just keep trying” and something feels off, advocate for yourself. Ask for a referral to a reproductive endocrinologist. When it comes to fertility, time is not something you get back.
The workup includes a semen analysis, ovarian reserve testing (AMH blood test and antral follicle count), imaging of the uterine cavity and fallopian tubes, and a hormonal panel including thyroid function. Even if everything was normal during your first pregnancy, it all needs to be reassessed: your body at 38 is not the same body it was at 33 (don’t I know it).
Treatment Options
Treatment depends on your specific diagnosis, age, and goals. Options range from lifestyle optimization and medicated IUI to IVF with preimplantation genetic testing (PGT). For patients 38 and older, ASRM considers it reasonable to go straight to IVF, which offers higher per-cycle success rates and the ability to screen embryos for chromosomal normality before transfer.
If you previously froze eggs or embryos, now may be the time to use them. That’s exactly what happened in my case: at 37, facing secondary infertility, those embryos I froze at 34 became my lifeline. Frozen eggs and embryos don’t age; they retain the reproductive potential of whenever they were frozen.
I’ve also seen patients told they needed donor egg who went on to conceive with their own eggs after finding the right team and the right lab. Persistence and strategy matter enormously. Not every story ends that way, but it’s important not to close doors prematurely.
The Bottom Line
Fertility is not linear. I’ve had patients who conceived their first child on a honeymoon and then spent two years and three IVF cycles trying for their second. I’ve had patients go the other direction: IVF for baby one, spontaneous conception for baby two. The only pattern is that there isn’t one, which is exactly why “it worked before” is not a diagnostic tool.
If something feels off, trust that instinct. Get the workup. Don’t let the fact that you already have a child talk you out of asking for help, or let anyone else talk you out of it, either. The earlier you get answers, the more options you have to work with.
If you’re navigating this right now, I’d love to hear from you — find me on Instagram. For a much deeper dive into everything we covered here, my book The Lucky Egg walks through the full diagnostic and treatment roadmap. And if you want my latest content delivered monthly, subscribe to The Lucky Egg Drop.