How to Increase Your Chances of Embryo Transfer Success?
The Embryo Transfer: this is the culmination of IVF treatment. The moment every patient eagerly awaits. The embryo may have been created and frozen in a prior IVF cycle, months or even years ago. Or it could be a ‘fresh’ embryo that developed a few days to a week after the egg retrieval procedure. Because of the work- the emotional investment, the financial burden of treatment, the attrition in numbers going from eggs to embryo, embryo transfer success always feels like a high stakes game. Success rates can approach up to 65-70% and depend on a wide variety of factors – mainly the embryo (is it genetically normal? Can it express its own genes properly?) and the uterine environment (is the lining of the uterus healthy and free of infection, fibroids, scar tissue, etc). The truth is, most fertility doctors believe the embryo transfer success is seldom related to what you do after the transfer (outside of taking your medications). Often, we cannot precisely pinpoint why some transfers work and others don’t – particularly when we are transferring embryos deemed to be genetically normal. Still, I think it is important for patients to prepare themselves adequately and feel that they have put their best foot forward before and after the transfer.
What to expect during an embryo transfer cycle: Preparing the uterus for transfer
If transferring a frozen embryo, we will use estrogen (usually oral and/or vaginal pills, but could also be patches or injections) for 1-2 weeks to thicken the uterine lining. These medications start after stopping birth control or on the 2nd or 3rd day of your period. We check the thickness of the uterine lining and if it is at least ~7mm thick, we will schedule the embryo transfer. We start progesterone (injections or a combination of oral and vaginal pills) for ~5 days leading up to the transfer date. We continue the estrogen and progesterone after the transfer up until the pregnancy test, which usually takes place 8-9 days later. If you are pregnant, these medications will continue for another 4-5 weeks until the placenta takes over production of these hormones.
If the embryo is being transferred in an IVF ovarian stimulation cycle (a week after egg retrieval), estrogen and progesterone are usually started after the egg retrieval.
It is also important to mention that some people will have a frozen embryo transfer done by tracking their natural menstrual cycle and having the embryo thawed out and transferred approximately a week after ovulation. Their doctor may decide to also give them medications, but generally fewer medications are used/needed in this scenario.
What happens during the Embryo Transfer procedure?
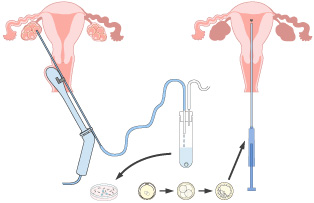
The transfer itself is a very quick, painless, and generally uncomplicated procedure. No sedation/anesthesia is required. We ask you to fill your bladder by drinking water 1-2 hours prior to the procedure. A full bladder allows us to get a clear picture on the sonogram (which is done abdominally) which guides us as we perform the transfer. We place a speculum in the vagina and clean off the cervix with some solution. An assistant uses gentle pressure on your lower abdomen with the ultrasound probe, so that we can get a side profile view of the uterus and visualize the catheter used to transfer the embryo. We will usually do a quick ‘trial run’ by passing a ‘test catheter’ through the cervical opening to make sure we can easily find the top of the uterine cavity (sometimes there can be a winding path to get there). Once we feel confident that we know ‘where to go’, we tell the embryologist to bring in the embryo from the lab next door. The embryo has been thawed out hours in advance of the transfer and is ready and waiting! They hand us the catheter loaded with the embryo inside, with a syringe attached to the end. We gently place the catheter in the cervix and snake the flexible tipped catheter to the top of the uterus and use the plunger of the syringe to deliver the embryo from the catheter to a few centimeters from the top of the uterine cavity. We then remove the catheter slowly and give it back to the embryologist who flushes it while checking under the microscope to confirm the embryo successfully left the catheter and was transferred into your uterus. We then take you to another room to relax for a little while and then empty your bladder and go home. The whole thing takes about 10 minutes!
Next comes the hardest part – the waiting game…
Patients always ask about what they can vs. can’t do after the transfer and how to maximize the chance of success. The truth is, you can’t really mess this up (if you take your medications). The most important crucial thing of all is to take your medications (estrogen and progesterone) to support the pregnancy, since the ovaries which normally do this in early pregnancy aren’t usually producing sufficient quantities of these hormones after an egg retrieval and in a frozen embryo transfer cycle where ovulation is not taking place.
There are many pieces of advice given to maximize embryo transfer success – some is rooted in scientific evidence, others in common sense and logic. There are also many myths which can lead to overly restrictive behaviors which can make a stressful process more torturous than it needs to be. This is why I wanted to summarize my personal DOs and DON’Ts that I like to share with my patients. *Remember, this is my opinion, and should not replace the advice of your doctor who knows your specific case – talk to your doctor and don’t go rogue and deviate from their instructions*
My list of DOs for Embryo Transfer Success:
Practice self-love: Be kind to yourself.
You are a badass for getting this far. You have put in the effort and work and deserve a break. Take it easy the day of your transfer and cut yourself some slack. Bed rest has not been shown to clinically improve outcomes, and of course being sedentary for long periods of time is never healthy. But you may want to clear your work schedule the day of your transfer to minimize stress and make the day easier to get through. You may also want to arrange your schedule/life so that you have space and time to take a few days to chill out after the transfer. Again, no study has shown that stress can cause an embryo transfer to fail. But removing all possible stressors and prioritizing rest and relaxation will definitely give your mental health a boost.
Take your medications and stay organized.
Taking estrogen and progesterone is extremely important to embryo transfer success and the development of an early pregnancy. If you need refills, ask the clinic in advance to call this in. Make every effort to not miss doses and to stay on top of things. Also know that if you do miss a dose, it is not the end of the world (ie. intramuscular progesterone stays in your system for more than 1 day)– but you should speak to your clinic to get advice on how to make up for the missed dose, if it is necessary.
Get at least 7-8 hours of sleep per night.
Sleep deprivation has been linked to lower pregnancy rates, in some studies. Lack of sleep can cause high cortisol levels and derange the hormonal environment. It also makes it harder to withstand stress and anxiety.
Act like you are pregnant.
Let’s assume the best – that the transfer worked and you are pregnant. This means avoiding alcohol, raw undercooked foods, toxic chemicals, and extreme temperatures (ie. sitting in a hot tub), and keeping caffeine intake to less than 200mg per day. It also means taking prenatal vitamins, wearing comfortable non-restrictive clothing, and maintaining a healthy diet low in processed carbs and high in protein and healthy fats.
My list of DON’Ts:
Don’t put anything in your vagina (other than progesterone) for the first few days after transfer.
This is to avoid the theoretical risk of introducing infection into the reproductive tract. Since the catheter entered the cervix to drop off the embryo, technically there was communication from the vaginal canal to the reproductive tract. Out of an abundance of caution, we tell women to not have sex in the first few days after a transfer. There is little to no evidence that having sex around the time of embryo transfer can impact success rates, but we give these instructions just in case.
Don’t ‘cheat’ and take a pregnancy test earlier than instructed.
This is by far the hardest advice to follow. After all, what’s the harm of peeing on a stick at home? First off, if you test even 1-2 days too early you may get a false negative reading, which says you aren’t pregnant when you truly are. This can happen because the embryo is not yet producing a meaningful level of the pregnancy hormone, beta-hCG, and/or because the home test being used is not sensitive enough to pick up the low level of hormone being produced at that early stage. Either way, it may devastate you for no reason when you actually are pregnant. And worse, some patients may opt to stop their medications supporting the pregnancy, without consulting their doctor, because they are falsely convinced they aren’t pregnant.
Don’t read too deeply into physical symptoms.
Lack of nausea 1 week after the transfer does NOT mean the transfer didn’t work. Nausea usually affects most pregnancies at 7-8 weeks and beyond. Also, if you feel cramps or have a bit of spotting, do not worry. If that embryo is implanting, there is a lot of remodeling going on inside that uterus, and some cramps and a little bleeding can be a totally normal part of the process. Let your doctor know if you have any bleeding, especially if you have a ‘negative’ bloodtype or if you don’t know your bloodtype (it is important for women with a negative blood type may need to receive an injection of antibodies if they have vaginal bleeding).
The wait is truly the hardest part. I recommend focusing on the DOs listed above, avoiding the DONTs, and setting yourself up for success by assembling your tribe – your network of friends/family/therapists who you can rely on to get you through this time. The week-long wait is best filled with conversations with people you can lean on for support, fun distractions like bingewatching your favorite Netflix show or movies, and healthy self-care.
Focusing on making the journey manageable, even enjoyable, is the best way to get to the destination, in this case our destination is a successful embryo transfer. If you are reading this because you are preparing for, or in the midst of an embryo transfer cycle, or in that dreaded waiting phase – I wish you the very best…congratulations on making it this far and good luck!
Dr. Lucky Sekhon
My name is Lucky Sekhon and I'm a double board-certified OBGYN, and Reproductive Endocrinologist & Infertility specialist practicing at RMA of New York. My mission is to empower women with practical and scientifically accurate information to make the right fertility decisions for themselves.
Follow me on Instagram to keep up to date with my fertility related posts and content.

