Understanding Dominant Follicle Selection and Ovulation in Fertility
Understanding ovulation and dominant follicle selection is the key to understanding so much about your reproductive system.
The process of selecting and ovulating a dominant follicle is known as folliculogenesis and ovulation, respectively. It is a complex process that involves the interplay of hormones and physiological changes within the ovary. Here is a simplified description of how a dominant follicle is selected and ovulated:
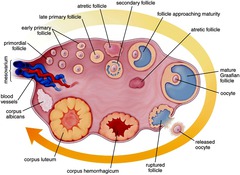
- Follicular Phase: The follicular phase of the menstrual cycle begins on the first day of menstruation and lasts until ovulation. During this phase, several follicles (fluid-filled sacs containing immature eggs) begin to develop within the ovaries.
- Follicle-Stimulating Hormone (FSH): At the beginning of the follicular phase, the pituitary gland releases follicle-stimulating hormone (FSH), which stimulates the growth of several follicles within the ovaries. Each follicle contains an immature egg (oocyte).
- Selection of the Dominant Follicle: As the follicles grow, they start to produce estrogen. Eventually, one follicle becomes larger and more active than the others, and it is referred to as the “dominant follicle.” The dominant follicle continues to produce increasing amounts of estrogen, which has a negative feedback effect on FSH production. As a result, FSH levels decrease, and the other follicles stop growing and undergo atresia (degeneration). The dominant follicle continues to grow and mature.
- Luteinizing Hormone (LH) Surge: The high levels of estrogen produced by the dominant follicle eventually trigger a surge in luteinizing hormone (LH) from the pituitary gland. The LH surge is a key event that initiates the final maturation of the egg within the dominant follicle and prepares it for ovulation.
- Ovulation: The LH surge causes the wall of the dominant follicle to weaken and rupture, releasing the mature egg (ovum) from the ovary into the fallopian tube. This event is known as ovulation. The released egg is now ready for fertilization by a sperm cell.
- Luteal Phase: After ovulation, the remnants of the dominant follicle transform into a structure called the corpus luteum, which produces progesterone to support a potential pregnancy. If fertilization does not occur, the corpus luteum degenerates, leading to a drop in progesterone levels and the onset of menstruation, marking the beginning of a new menstrual cycle.
Overall, the selection and ovulation of the dominant follicle are regulated by a complex interplay of hormones and physiological changes within the ovary. The process is cyclical and occurs approximately once a month in women of reproductive age.
With PCOS, the pituitary is sending FSH and LH signals to the ovary but the ovary has a sort of resistance to these signals. In people with high prolactin levels, pituitary problems (after surgery, a major hemorrhage, brain injury), or who expend more calories than what they take in (professional athletes, patients with anorexia etc), the pituitary can have a deficiency of FSH and LH and this is what causes ovulation to not occur and periods to be absent. Medications like clomid/letrozole work by fooling the pituitary gland into thinking there is not enough estrogen so that it churns out higher levels of FSH and LH to force the ovary to select one or more follicles to become mature/dominant and release one or more eggs. Hormonal contraception like birth control pills work by suppressing the release of FSH and LH from the pituitary to prevent ovulation. When you get a period while on birth control pills it is merely a ‘fake period’ which means breakdown of the uterine lining due to the withdrawal of birth control hormones for 1 week – this is not bleeding because of a recent ovulation.
Understanding how ovulation happens, can help you better understand the fertile window (when to try) and the mechanism behind certain medical conditions and medications that can cause irregular/absent ovulation and periods.