‘Difficult’ embryo transfers: how to prevent them and optimize the chance of success
(And a true story of a time I successfully overcame an unexpectedly challenging transfer!)
For fertility doctors, the embryo transfer is that ‘do or die’ high-stress, high-stakes moment where you want to get everything PERFECT.
Thankfully, most embryo transfers are very straight forward – they typically take 5-10 minutes to perform, and are usually painless and do not require anesthesia. Every once in a while, an embryo transfer will be difficult – there are ways to anticipate this in advance and to prepare for challenges and optimize things before the embryo transfer day.
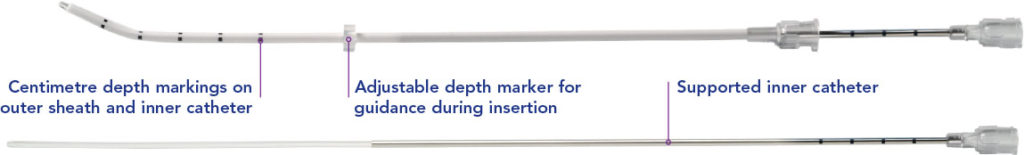
I am meticulous in my preparation in the lead up to an embryo transfer. I make sure that a catheter has been passed through the cervical canal and to the top of the uterus at least once in the few months leading up to the transfer, whether it be during IUI, a saline sonogram, a HSG, or other type of procedure involving the uterine cavity. If the cervix is narrow or winding and it is really challenging to get to the top of the uterus, I know I will either need to dilate the cervix in a minor procedure prior to the transfer cycle itself or use special tools (ie. rigid catheters) at time of transfer.
It is also important to figure out a patient’s comfort level. Embryo transfers are not typically done under anesthesia/sedation as they are quick and painless and relatively simple procedures for most patients. If a patient has a pelvic floor issue like vaginismus (an involuntary spasm of pelvic floor muscles which can lead to an inability to tolerate a pelvic/speculum exam) this can obscure the view of the cervix and make doing a transfer challenging. It can be helpful to premedicate with relaxing meds beforehand and in extreme cases I have done embryo transfers under sedation administered by an anesthesiologist.
BEFORE the embryologist thaws out the embryo for transfer, I need to KNOW that the uterine cavity is perfect and that the path to the top of the uterine cavity is straight-forward to navigate. I make sure I know which type of catheter and the degree of the curve of the cervix so that the transfer is sure to be easy. An easy, quick transfer is more likely to succeed that a challenging one that takes several tries and involves excessive manipulation of the inner cervix and path to the uterus – which can lead to bleeding, swelling, and irritability of the uterus (which is a big muscle that can spasm/contract).
A story about the most difficult transfer I have ever done:
**(Spoiler Alert: it was difficult, BUT ultimately was a success!!)**
I have a distinct memory from 5 years ago of an unexpectedly challenging transfer. It is one thing to go into a transfer anticipating certain challenges because you know based on a prior ‘catheter check’ that the cervix is narrow or winding, or that there is difficult visualization of the uterus due to fibroids etc. But this was a case where I had done a recent saline sonogram and it was really easy to find the top of the uterus and visualize everything- I never anticipated any difficulty. Cut to the day of the actual transfer– It was a day where I had several transfers to do and all was going smoothly. I was in the zone. I was in a great groove and things were going very smoothly for each case.
My patient was a 40 year old with a single euploid embryo with a perfect grade – this was the only normal embryo she had and was able to make. She wanted 1 child – and this embryo was IT. No pressure, right?
So I sat down and snapped into my routine. When I began to do the trial run (a quick check before the embryologist brings the actual loaded embryo transfer catheter in), the cervical canal not only felt more narrow and constricted than what I had recalled from the saline sonogram a month prior but also it was sharply curved and took a winding path. I did not panic. I did what I know to do – I systematically went through my checklist of tools and strategies. I used the ultrasound to navigate and figure out the best path forward. It became clear after a few attempts, I would need a more rigid catheter. When I switched to different catheters with increasing levels of rigidity and still couldn’t get anything past a certain point in the cervical canal, I “phoned a friend” and asked one of my trusted colleagues and mentors to come into the room and sit down and try the path to the top of the uterus with a rigid catheter. He also felt it was impossible to advance the catheter beyond a certain point. This is when I began to feel a little stressed. I have never *not* been able to do a transfer before and this was the patient’s only embryo and I really did not want to resort to refreezing it because we could not complete the transfer. I also felt so bad for the patient as she was being so patient and understanding but had been on the exam table, legs in the stir ups with a full bladder, for far too long.
I gave her a break. We told her to go empty her bladder and sit in a recliner in the recovery room. I moved on and did a few other transfers for patients who were scheduled after her. Meanwhile, she took a rest and began to refill her bladder by drinking more water.
I finished the rest of my patients’ transfers without incident – all went smoothly… so I circled back to my patient with the impossibly difficult cervix and we brought her back in the room.
Now I don’t know if it was that the bladder was refilled the perfect amount, or the change in position of the patient on the bed – whatever happened when she went to empty her bladder and hang out in the recovery room, her anatomy shifted and I was able to get the catheter in and complete her transfer.
And GUESS WHAT?! – 9 days later, she was pregnant and ended up having a healthy girl 9 months later!
This difficult transfer sticks out in my mind because it is a rare example of a time when I had ZERO anticipation that the transfer would be challenging. It was a major lesson that the cervix’s position can change – things can change. Change is the only constant. And while it is important to do whatever we can to prepare for the important moments, like embryo transfer, we need to stay open-minded and flexible and be able to adapt to new conditions and when new information is presented to us. And at the end of the day, if the transfer for some reason becomes very challenging, you should never be afraid to ask your colleagues for help or to make the difficult decision of refreezing the embryo so that the transfer can occur when conditions are perfect.
I am so grateful that my patient’s difficult embryo transfer could be completed after all and that it was a success for my patient.
My advice to anyone going through an embryo transfer cycle:
You should prepare by coming in with a full bladder (this helps to straighten out the cervix and make for an easier path to the top of the uterus) and to ensure you have had imaging of the uterine cavity within the past ~6-12 months or sooner and that all concerns (ie. polyps, scarring etc) have been addressed. If you have a history of pelvic floor disorders/tension and have a hard time tolerating speculum exams, consider pelvic floor PT and asking your doctor to prescribe a relaxing agent like valium, for example. In extreme cases, embryo transfers CAN be done under anesthesia. Always consult with your doctor about these types of concerns and your potential options BEFORE embryo transfer day.