Platelet-Rich Plasma (PRP) for Ovarian Rejuvenation: Hype or Hope?
If you’ve been exploring fertility treatments, you may have come across Platelet-Rich Plasma (PRP) as a supposed “ovarian rejuvenation” therapy—a method that claims to improve egg quality and increase fertility in women with diminished ovarian reserve, premature ovarian insufficiency, or even menopause. At first glance, it sounds revolutionary: using your body’s own growth factors to turn back the biological clock. Clinics offering PRP promote it as a cutting-edge solution for those struggling with age-related infertility, but does the science actually support these claims?
The truth is, PRP for ovarian rejuvenation is still highly experimental, and the data doesn’t back up the hype. While some studies suggest PRP can temporarily increase AMH levels (a marker of ovarian reserve), there’s no solid evidence that it improves egg quality, embryo development, or pregnancy rates.
My name is Dr. Lucky Sekhon, and I’m a Reproductive Endocrinologist and Infertility Specialist (REI) based in New York City. When I’m not busy helping my patients build their families, I use my platform on Instagram and this blog to demystify the fertility journey and cut through the misinformation that often overwhelms those trying to conceive. If you find this blog helpful, I encourage you to follow me on Instagram (@lucky.sekhon) or sign up for my free monthly newsletter for science-backed fertility insights, expert advice, and real talk about reproductive health.
In this blog, I’ll examine what PRP is and its mechanisms, evaluate the current research on PRP for ovarian rejuvenation, and explain why it hasn’t proven to be an effective fertility treatment. Let’s dive into whether this experimental treatment is worth your investment or if it’s simply another over-hyped fertility trend.
What is Platelet-Rich Plasma (PRP) and Why Do Some Believe It Can Help with Ovarian Rejuvenation?
The idea of ovarian rejuvenation is exciting. The concept that we could reawaken aging ovaries and potentially improve fertility using the body’s own healing factors is undeniably appealing. Platelet-Rich Plasma (PRP) has been widely used in medicine for decades—helping to repair injuries, speed up wound healing, and even stimulate hair growth. It’s no surprise that reproductive medicine has turned its attention to PRP, asking: Could this same regenerative technology help women with diminished ovarian reserve (DOR), premature ovarian insufficiency (POI), or even menopause?
At first glance, it’s an intriguing possibility. If PRP has been shown to stimulate tissue regeneration and cell growth in other areas of the body, why not in the ovaries? Some fertility clinics have begun offering ovarian PRP injections, claiming that it could activate dormant follicles, improve egg quality, and even boost ovarian reserve.
How is PRP Prepared and Used in Fertility Treatment?
The PRP process begins with a simple blood draw, just like you would have done for routine lab work. The blood is then placed in a centrifuge, which spins at high speeds to separate the platelet-rich plasma from the red blood cells. The resulting PRP contains high concentrations of growth factors and cytokines, which are thought to promote cellular regeneration and tissue repair.
Once the PRP is prepared, it is injected directly into the ovaries through a vaginal ultrasound-guided procedure—similar to how eggs are retrieved during IVF. The hope is that these growth factors will rejuvenate ovarian tissue, encouraging the recruitment of more follicles and improving overall ovarian function.
This idea—harnessing the body’s own healing properties to enhance fertility—is an exciting one. But ideas and excitement only go so far, and at the end of the day, the efficacy of this treatment can only be shown through rigorous scientific data, so let’s see what the science says.
What the Studies Say: PRP for Ovarian Function and Pregnancy Rates
For years, the data on Platelet-Rich Plasma (PRP) for ovarian rejuvenation was limited to small observational studies and case series-essentially, clinics documenting their experiences with a handful of patients and reporting what happened after the treatment. These studies lacked control groups, meaning there was no way to determine whether PRP actually made a difference or if the changes seen were simply due to normal fluctuations in hormone levels. While some reports showed temporary increases in AMH levels or follicle counts, these effects appeared to be transient and not linked to better pregnancy rates. A major theory is that mechanically disrupting the ovarian tissue and follicles releases stored AMH into the bloodstream, leading to a short-term rise that does not reflect true, long-lasting improvement in ovarian reserve.
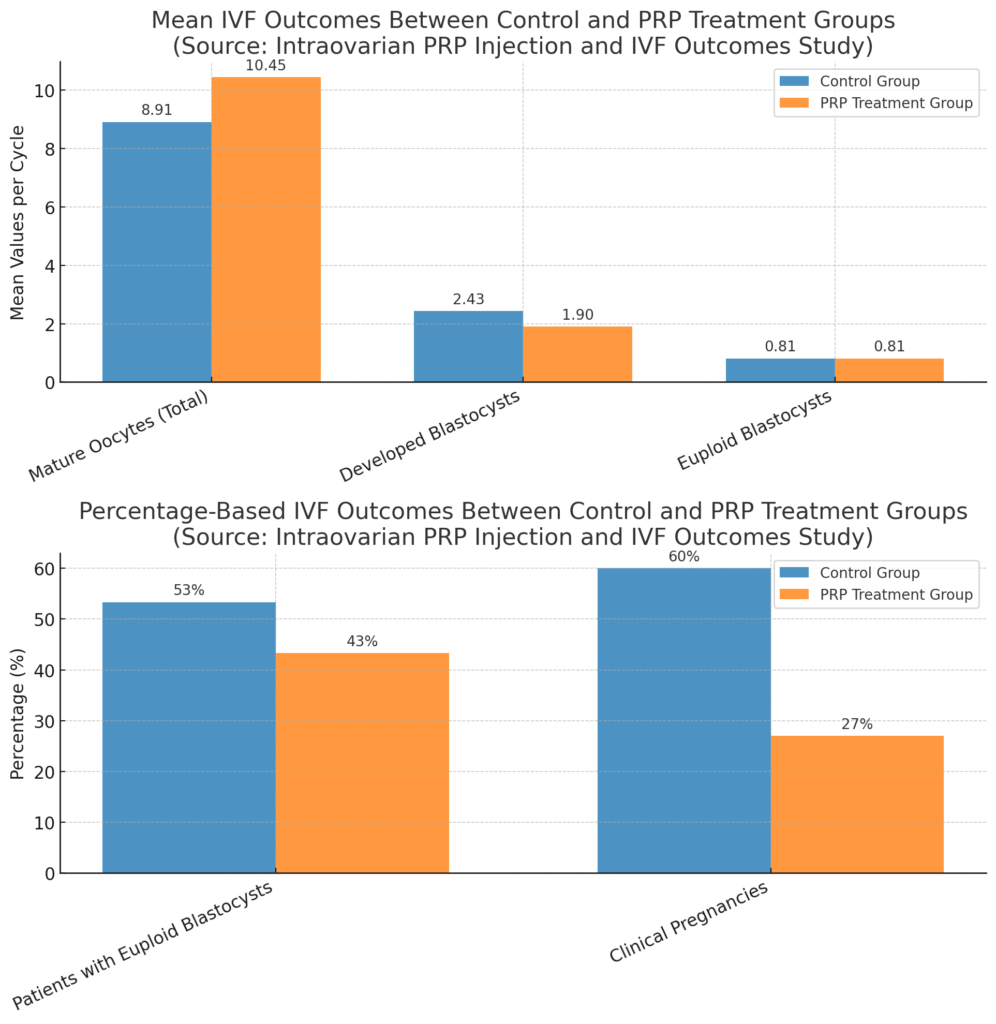
In 2024, two randomized controlled trials (RCTs) finally put PRP to the test against a control group (one of which received a placebo. In the first study, while PRP led to a slight increase in the number of eggs retrieved (10.4 vs. 8.9 in controls), it had no impact on the number of genetically normal embryos, and surprisingly, the pregnancy rate was significantly lower in the PRP group (27% vs. 60%).
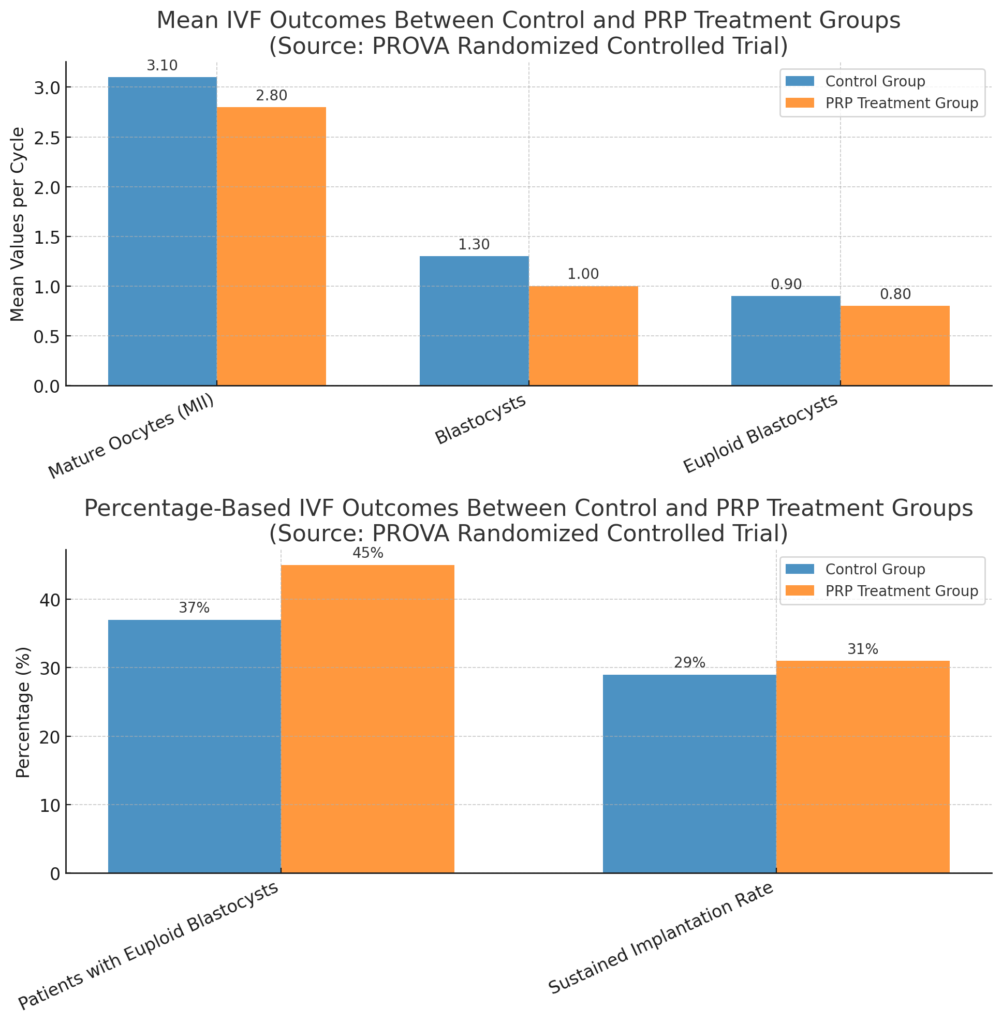
The second study, a larger multi-center trial, found no statistically significant difference in ovarian reserve, fertilization rates, or pregnancy outcomes between those who received PRP and those who did not, despite small numerical differences in the observed data favoring PRP.
Together, these trials show that PRP does not enhance fertility and may even have a negative effect on outcomes. Unlike earlier studies, which were often limited by small sample sizes, retrospective designs, or lack of proper controls, these randomized controlled trials (RCTs) eliminate many sources of bias and confounding. As the gold standard in clinical research, RCTs randomly assign participants to treatment or control groups, ensuring that any observed differences are truly attributable to the intervention rather than external factors. The consistency of findings across these rigorous studies strengthens confidence in the conclusion that PRP does not improve fertility outcomes.
Is PRP Worth the Hype? My Perspective
I understand the deep, all-consuming desire to do everything possible to improve your chances of getting pregnant. When you’re struggling with infertility, every option—especially one that feels innovative and promising—seems worth considering. The idea that a simple injection of platelet-rich plasma (PRP) into the ovaries could improve egg quality and boost IVF success is incredibly appealing. I get why so many patients are asking about it.
But here’s what I want you to know—PRP remains experimental. Despite the excitement surrounding it, there is no reliable evidence that PRP improves ovarian function, egg quality, or pregnancy outcomes. The best-designed studies we have—rigorous, gold-standard randomized controlled trials—have shown no meaningful benefit.
I am not against trying experimental therapies. If you have the financial means and feel strongly about trying it, I understand why you might want to pursue it. Sometimes, doing something—even if the science isn’t fully there—can help you feel like you’re leaving no stone unturned. But I also urge you to be aware of its experimental nature and that there are possible risks due. Be wary of clinics promoting PRP as a miracle cure, especially for women with advanced age over 45. Fertility treatment is already filled with uncertainty, and the last thing I want is for patients to invest their hopes, time, and money into something that isn’t backed by strong evidence.
The truth is, the most precious resource in fertility treatment isn’t money—it’s time. Unlike financial resources, which can be replenished, time is something none of us can get back. Every cycle spent on an unproven treatment is a cycle that could have been spent on approaches with stronger evidence behind them. PRP falls into the same category as other treatments such as Omnitrope, which I previously wrote about, an add-on that is not likely to do harm, but also, just as unlikely to alter your outcomes.
I wish PRP was the breakthrough we’re all searching for. If the data showed clear and consistent benefits, I would be the first to recommend it. But right now, the science just doesn’t support it. If you’re considering PRP, I encourage you to weigh the hope it offers against the costs and time it may take away—because in the end, making the most of every cycle is what truly matters.
I’m Dr. Lucky Sekhon, a board-certified Reproductive Endocrinologist and Infertility Specialist. My mission is to empower people with the knowledge they need to take control of their fertility journeys—whether they’re just starting to think about their future family or are in the thick of treatment. Through my practice, my blog (Lucky Egg), and my social media platforms, I share science-backed, honest, and compassionate guidance to help you navigate the often overwhelming world of fertility. Because when it comes to making informed decisions about your reproductive health, knowledge is power—and time is everything. You can find me on Instagram, TikTok, and YouTube for more fertility education, insights, and support.
References
Herlihy NS, Cakiroglu Y, Whitehead C, et al. Effect of intraovarian platelet-rich plasma injection on IVF outcomes in women with poor ovarian response: the PROVA randomized controlled trial. Hum Reprod. Published online May 9, 2024. doi:10.1093/humrep/deae093.
Barrenetxea G, Celis R, Barrenetxea J, et al. Intraovarian platelet-rich plasma injection and IVF outcomes in patients with poor ovarian response: a double-blind randomized controlled trial. Hum Reprod. 2024;39(4):760-769. doi:10.1093/humrep/deae038.
Li X, Liu H, Lin G and Xu L (2023) The effect of ovarian injection of autologous platelet rich plasma in patients with poor ovarian responder: a systematic review and meta-analysis. Front. Endocrinol. 14:1292168. doi: 10.3389/fendo.2023.1292168.
Pacu P, Pacu I, Pacu A. Intraovarian injection of autologous platelet-rich plasma in patients with low ovarian reserve: Effects on ovarian function and reproductive outcomes. J Clin Med. 2023;12(17):5292. doi:10.3390/jcm12175292.
Sfakianoudis K, Simopoulou M, Nitsos N, et al. A case series on platelet-rich plasma revolutionary management of poor responder patients. Gynecol Obstet Invest. 2019;84(1):99-106. doi:10.1159/000491697.
Sills ES, Wood SH. Autologous activated platelet-rich plasma injection into adult human ovary tissue: Molecular mechanism, analysis, and discussion of reproductive response. Reprod Biol Endocrinol. 2019;17(1):72. doi:10.1186/s12958-019-0517-9.

