Growth Hormone and False Promises: The Truth About Omnitrope in IVF
When it comes to IVF, some treatments like Omnitrope, an injectable form of human growth hormone, often take on a life amidst their hype, becoming the subject of endless questions, online debates, and whispered hopes in clinic waiting rooms. It’s no surprise that so many of my patients ask me about it.
My name is Dr. Lucky Sekhon, and as both a practicing REI and IVF patient, I get it, when you’re navigating the emotionally and financially intense world of IVF, anything that might promise to improve egg quality or embryo development is tempting to consider. But here’s an important truth: just because a treatment might help doesn’t mean it’s the right choice for you, or that it should automatically be added onto the pile “just to be safe.” There are very real medical, financial, and practical considerations to weigh, especially when it comes to something as complex and deeply personal as IVF.
I practice medicine based on a simple tenet, that treatment options need to be backed by hard science, not gut feelings, anecdotal findings, or what ‘just makes sense’. Any treatment I recommend to my patients must earn its place in my fertility protocol quiver, not through hype or hopeful speculation, but rather through rigorous, high-quality evidence.
In this post, I want to demystify Omnitrope and explain why I don’t use Omnitrope in my practice (outside of patients with growth hormone deficiencies) and help you better understand the scientific evidence, or lack thereof, behind this controversial treatment.
What Is Omnitrope and Why Is It Used in IVF?
Omnitrope is a brand of human growth hormone (hGH) that has gained traction as a potential add-on treatment in IVF. Human growth hormone is a naturally occurring hormone produced by the pituitary gland, and its primary role is to stimulate growth, cell regeneration, and metabolism. When used in the context of IVF, Omnitrope is typically administered as a daily injection in the lead-up to and during ovarian stimulation. The hope is that it will improve ovarian response to stimulation medications, enhance egg quality, and ultimately result in better embryo development.
The scientific basis for its use lies in its interaction with insulin-like growth factor-1 (IGF-1). hGH stimulates the liver to produce IGF-1, which in turn plays a role in promoting follicle growth and development by enhancing the response of the ovaries to follicle-stimulating hormone (FSH). This mechanism has led to the hypothesis that growth hormone supplementation could be beneficial for patients undergoing IVF, especially those with poor ovarian reserve or prior suboptimal responses to stimulation.
In fact, women with known growth hormone deficiency, a rare condition effecting ~0.025% of women, are more likely to experience infertility. Studies have shown that correcting this deficiency with growth hormone supplementation can improve reproductive outcomes. This observation has driven curiosity about whether administering growth hormone might also help women without a diagnosed deficiency during IVF?
The Evidence: What Science Says About Omnitrope in IVF
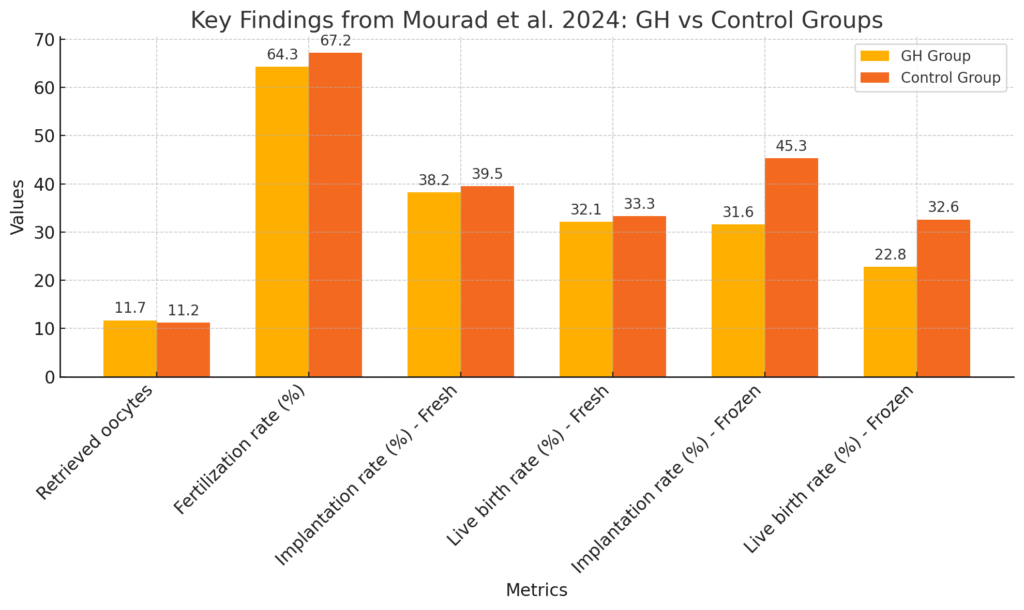
One of the major reasons I haven’t incorporated Omnitrope in my treatment protocols is the fact that there are no well-designed study that demonstrates that Omnitrope makes a meaningful difference in IVF outcomes. While smaller studies (Sood et al. 2021) and meta-analyses hinted at possible benefits for certain groups, like poor responders, the data was inconsistent and inconclusive. But just last month, a landmark study, aptly titled “Empirical use of growth hormone in IVF is useless: the largest randomized controlled trial”, was published in Human Reproduction that provided the clearest picture we’ve had so far. This randomized controlled trial, the gold standard in scientific investigation, involving 288 patients expected to have a normal ovarian response, found no differences in the number of eggs retrieved, fertilized, or reaching the blastocyst stage between those who received human growth hormone injections and those who didn’t. Pregnancy and miscarriage rates were also the same between the two groups.
For me, this study was a game-changer in confirming what I’ve observed in my own practice: Omnitrope doesn’t deliver on the promises it’s often associated with. While earlier, small studies suggested small improvements in metrics like egg numbers for poor responders, there’s never been any solid proof that it using omnitrope as an adjunct in IVF actually moves the needle and improves outcomes like live birth rates—the outcome that matters most. Prior to this study’s publishing, I didn’t recommend Omnitrope because of a lack of reliable scientific data, as well as the potential risks and expense (which I’ll get into later). This new evidence has only reinforced my stance and backs it up with real scientific data to show that Omnitrope has no measurable benefit in IVF outcomes for women and should not be recommended as part of fertility treatment, outside of treating growth hormone deficiency.
Risks and Downsides: The Cost of Omnitrope in IVF
Adding Omnitrope to an IVF protocol isn’t without consequences, and it’s important to weigh both the financial and medical risks before committing to it. One of the biggest downsides is cost. Growth hormone injections are expensive, often adding several thousand dollars to an already costly process. For many patients, this extra expense can make IVF even less accessible, especially when the evidence doesn’t clearly show it improves outcomes in a meaningful way.
Beyond the financial burden, there are potential side effects to consider. While short-term use of growth hormone is generally safe, it can cause issues like fluid retention, joint and muscle pain, and carpal tunnel syndrome. Less common but more serious risks include high blood sugar, pancreatitis, and even the potential for cancer recurrence in patients with a history of tumors. Long-term use has been linked to conditions like irreversible acromegaly, diabetes, and heart disease. While these side effects are rare, they’re a reminder that no medication is risk-free, and “just to be safe” isn’t always safe—or wise.
There are also legal and regulatory concerns. In the U.S., it’s illegal to prescribe growth hormone for off-label uses like infertility because it’s not FDA-approved for this purpose. While some clinics still offer it, this falls into a regulatory gray area that raises questions about its routine use. Given the high costs, the potential for side effects, and the lack of compelling evidence that Omnitrope improves IVF outcomes, I simply don’t believe it’s worth the risk. Until more robust data shows clear, meaningful benefits, it’s not something I recommend in my practice.
Making Informed Choices for IVF Treatments
I believe that when it comes to IVF, or any medical intervention you are considering, every medication or treatment added to your protocol should be grounded in strong, evidence-based science. Despite the buzz around Omnitrope, the most rigorous data we have shows that it doesn’t improve outcomes that truly matter, like pregnancy or live birth rates. While it’s understandable to want to try everything “just in case,” the risks, costs, and lack of proven benefit make it a treatment I can’t recommend in good conscience. My goal is always to offer care that balances hope with hard evidence, and for now, Omnitrope simply doesn’t meet that standard. As a fertility doctor who works at one of the nation’s premier IVF centers with the highest live birth rates per every patient who walks through our clinic doors seeking treatment, I can tell you that none of the 5000+ egg retrieval cycles performed each year involve the use of Omnitrope. Given the track record for IVF success and lab quality where I work, if the data and clinical experience added up to a point where proven benefits outweighed the downsides, we would surely begin to use growth hormone to maximize clinical success- but until that day, when patients ask me about Omnitrope, the answer remains: “Omni-NOPE!”.
As you navigate your own IVF journey, I encourage you to ask questions and make informed choices about the treatments you pursue. What does the research say? How does this intervention align with your specific needs? Are the risks and costs justified by clear benefits? IVF is a deeply personal and emotionally charged process, but it’s also a medical journey that deserves thoughtful, science-based decisions. Adding treatments without solid evidence can create unnecessary financial strain or medical risks that don’t move you closer to your goal.
You deserve a plan that’s tailored to you, one that prioritizes proven methods and gives you the best chance of success while balancing the practical realities that IVF treatment comes with. My name is Dr. Lucky Sekhon, and I’m a fertility specialist based in New York City. Through this blog and my Instagram, I share content focused on fertility and women’s reproductive health to help you make informed decisions about your care. If you’d like to stay updated on my latest insights and resources, I invite you to sign up for my monthly newsletter, The Lucky Egg Drop. And if you’re struggling with infertility and interested in booking a consultation with me at my New York office, please submit an appointment request here.