Embryo Grading and How It Influences IVF Outcomes
Embryo grading plays a pivotal role in the IVF process, offering insights into the potential success of an embryo transfer. This grading system, known as morphology grading, correlates with an embryo’s likelihood of implantation and culminating in a live birth. That’s right – your embryos get a ‘report card’ of sorts – and the scores can help us to select the best embryo for transfer. Selecting the best embryo does NOT mean choosing the embryo that will turn into the healthiest child, or the child that will get into an Ivy League school.
In this article, I will breakdown the following:
- Explain the different grading used to evaluate day 3 and blastocyst embryos.
- Break down the components of the morphology grading for an embryo and highlight their relative importance to IVF success.
- Show, via example, how I interpret different blastocyst morphology grade.
- Explain the interplay between embryo morphology and an embryo’s speed of development.
I have also recently launched my newest tool on the LuckyEgg blog, the AI-powered Euploid Embryo Predictor Tool. If you have ever asked yourself or your RE “what are the chances of producing a euploid embryo during my IVF cycle?”, then you should definitely check out this tool.
Grading Day 3 Embryos: The Cleavage Stage
When attempting to grade a day 3 embryo you do not use the same scale that blastocyst embryos (day 5) do. A day 3 embryo can undergo only a limited assessment, since at this stage of development the embryo is still relatively simple – it hasn’t yet differentiated into the two major cell types seen at day 5 and beyond, when the embryo turns into a ‘blastocyst’. The main things you can assess about a day 3 embryo are:
- Number of Cells: For a day 3 embryo, this can range from 3-4 cells up to 12-15 cells. In general, having an embryo with 8 or more cells suggests it is growing at a ‘normal’ pace – speed of embryo development is strongly correlated with reproductive potential
- Fragmentation: The percent of the embryos’ cells with fragments is thought to be a quality indicator. Fragments form in the embryo when there is unequal division of cells. Fragments are considered the ‘junk’ of the cell, and are likely not useful to the embryo. The higher the degree of fragmentation, the lower the chance of a pregnancy from a given embryo.
Grading Day 5+ Embryos: The Blastocyst Stage
By day 5, the embryo has evolved into a more complex structure known as a blastocyst, containing hundreds of cells divided into an inner cell mass (ICM) that will become the fetus and a surrounding layer called the trophectoderm, which will form the placenta. The grading criteria at this stage, which is known as the Gardner Schoolcraft grading system, become more detailed focusing on the following three major components: assessing the blastocyst’s expansion, quality of the inner cell mass (ICM), and the trophectoderm.
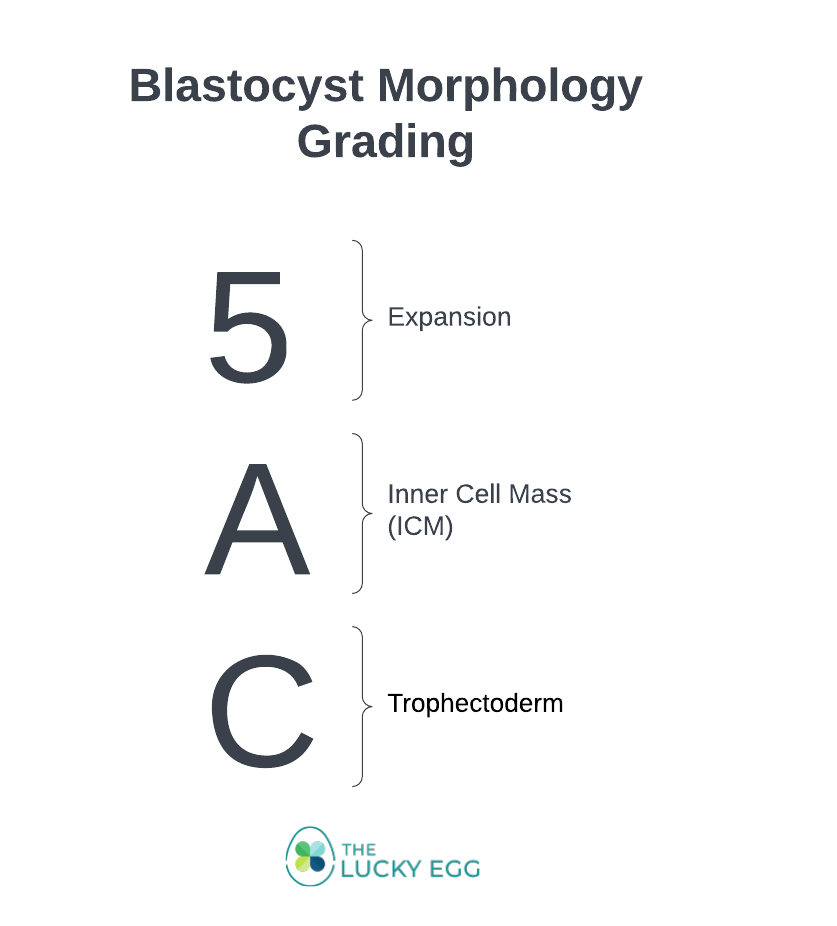
Expansion
The first digit in the embryo grade refers to the blastocyst’s expansion level, which ranges from 1 to 6. Expansion assesses the size of the blastocoel, the fluid-filled cavity within the blastocyst, and the thinning of the zona pellucida (the outer shell). This metric is crucial because it reflects the embryo’s ability to grow and expand, an essential step for implantation.
| Expansion Grade | Description |
| 1-2 | Early blastocyst, with a blastocoel less than half the volume of the embryo. |
| 3 | The blastocoel fills more than half of the embryo. In general, any embryo that can be frozen/biopsied for PGT must be at an expansion grade of 3, at a minimum. |
| 4 | A full blastocyst with a blastocoel completely filling the embryo. |
| 5 | A full blastocyst with a blastocoel completely filling the embryo. |
| 6 | Hatched blastocyst, where the embryo has broken free from the zona pellucida. |
Is a Higher Expansion Grade Always Better?
While a higher expansion grade is generally better, it is not an absolute. For example, an expansion grade 6 is not necessary better than a 4 or 5. An expansion level 6 embryo, one that is fully hatched, is theorized to be slightly more delicate and some data suggests there may be a lower ability to withstand the freezing and thawing process successfully. In general 4 vs. 5 vs. 6 will not be a gamechanger when it comes to the chances of implantation.
Inner Cell Mass (ICM)
The second part of the grading, denoted by the first letter (A-D), evaluates the inner cell mass, the group of cells that will develop into the fetus. The ICM’s quality is indicative of the embryo’s potential to develop into a healthy baby and is generally considered the most predictive of implantation and birth. The grades range from A to D – just like in school, As and Bs are preferred to Cs and Ds.
| ICM Grade | Description |
| A | Many cells that are tightly packed together. |
| B | Several cells that are loosely grouped. |
| C | Few cells, very loosely grouped. |
| D | Very few cells, if any. |
Trophectoderm
The third component, evaluated by the second letter (A-D), examines the trophectoderm, the cells that will form the placenta and support the embryo’s growth. The quality and organization of these cells are crucial for the embryo’s ability to implant and sustain a pregnancy. While the ICM grade is more predictive of implantation success, the quality of the trophectoderm is still essential for the overall health and development of the embryo. Similar to the inner cell mass, grades of A to D are assigned to the trophectoderm. As and Bs are better than Cs and Ds.
| Trophectoderm Grade | Description |
| A | Many cells forming a cohesive layer. |
| B | Several cells with slight irregularity in arrangement. |
| C | Few cells with loose organization. |
| D | Very few cells, poorly organized. |
Deciphering Blastocyst Grading: A Closer Look Embryo Evaluation
Blastocyst grading is a nuanced process that provides significant insights into an embryo’s potential for implantation and development into a healthy pregnancy. The grading is typically represented by a combination of numbers and letters, each indicating specific characteristics of the blastocyst. Here’s some examples to help you understand an few different grades and what they signify about an embryo’s quality:
| Grade | Expansion (1-6) | Inner Cell Mass (A-D) | Trophectoderm (A-D) | Interpretation |
|---|---|---|---|---|
| 5AA | Fully expanded blastocyst with a large fluid cavity and thinned zona pellucida | High-quality with many cells tightly packed | High-quality with many cells forming a cohesive layer | Excellent potential for implantation and development into a healthy pregnancy |
| 4AA | Moderately expanded blastocyst with a discernible fluid cavity | High-quality with many cells tightly packed | High-quality with many cells forming a cohesive layer | Very good potential, slightly less expanded than 5AA but with excellent cell quality |
| 5AC | Fully expanded blastocyst with a large fluid cavity and thinned zona pellucida | High-quality with many cells tightly packed | Lower quality with fewer cells and/or loose organization | Good potential for implantation, though concerns with trophectoderm may affect placental development |
| 4AC | Moderately expanded blastocyst with a discernible fluid cavity | High-quality with many cells tightly packed | Lower quality with fewer cells and/or loose organization | Good potential, but with possible limitations due to the trophectoderm quality |
| 3AA | Early blastocyst with a small fluid cavity | High-quality with many cells tightly packed | High-quality with many cells forming a cohesive layer | Good implantation potential, though less expanded than higher grades |
| 3CC | Early blastocyst with a small fluid cavity | Lower quality with fewer cells and/or loose packing | Lower quality with fewer cells and/or loose organization | Lower potential for implantation and development |
Understanding Blastocyst Grading in IVF Outcomes
The grading of blastocysts provides critical information for selecting the most viable embryo for transfer during an IVF cycle. Higher grades like 5AA indicate excellent potential for implantation and a successful pregnancy. However, even embryos with lower grades can result in successful pregnancies, underscoring the importance of individualized patient care and embryo selection strategies.
Embryos graded with higher scores for both inner cell mass and trophectoderm, such as ‘AA’, suggest a better quality embryo with a higher chance of successful implantation and pregnancy. Conversely, embryos with lower scores in these areas (‘C’ or ‘D’) may have reduced potential but are still considered for transfer based on the overall context of the IVF cycle and patient-specific factors.
The Interplay Between Embryo Development Speed and Morphology Grading
In the context of IVF success, it’s important to understand that the speed of embryo development can sometimes play a more decisive role than the embryo’s morphology grade alone. Embryos that develop rapidly and reach key milestones ahead of their counterparts might have a higher implantation potential, even if their morphology grading isn’t perfect. This aspect highlights the dynamic balance between the quality of the embryo (as assessed by morphology grading) and its developmental velocity.
Rapidly developing embryos are often a sign of robust biological vitality, suggesting they might overcome slight imperfections in cell arrangement or expansion grade. Consequently, an embryo that reaches the blastocyst stage by Day 5 may be favored over a Day 6 or Day 7 embryo with a comparable or slightly better morphology grade.
A Practical Example: Which Embryo Is the ‘Best’?
Consider the following scenario with embryos at different stages and with varying morphology grades:
- Day 5, Grade 4BB: A moderately expanded blastocyst with good quality inner cell mass and trophectoderm.
- Day 6, Grade 5AA: A fully expanded blastocyst from the following day with excellent quality in both inner cell mass and trophectoderm.
- Day 7, Grade 5AA: Similarly, a fully expanded blastocyst with excellent quality, but developed two days later than the Day 5 embryo.
In terms of which embryos have the greatest chance of success, the conventional wisdom might suggest prioritizing based on morphology grade alone (favoring the 5AA grades). However, considering the critical role of development speed, the Day 5, Grade 4BB embryo might actually be given precedence for transfer over the Day 6 and Day 7 embryos, even with their higher morphology grades. This prioritization reflects the empirical observation that earlier development can indicate a higher likelihood of implantation and successful pregnancy, potentially outweighing the pure morphology grading. This practical comparison underscores the nuanced approach needed in selecting embryos for transfer. Fertility specialists weigh both the speed of development and the detailed morphology grading, balancing these factors to optimize the chances of a successful IVF outcome.
How to Use Morphology Grading in Your IVF Journey?
Whether or not you genetically tested your embryos, we can use the grades to choose which embryo to use first. For patients with multiple embryos to choose from, we can pick the fastest embryo with the best grade. For those who only have 2-3 embryos and they know they want to have 2 children, I have had some patients ‘game the system’ and preferentially choose the ‘worst’ embryo with the lowest chance of success to be the first to be used for transfer. This way, if it works, the two better embryos can be reserved for future use, versus leaving the embryo with the lowest chance of success for the future, when egg quality/quantity would have likely declined, lowering the chance of being able to make more embryos in the future.
What strategy to use depends on how many embryos you have, and your family building goals, including when you plan to use the embryos in the future and what that means in terms of your age and projected egg quantity/quality. This is a conversation you should be having with your RE as they can provide expert guidance, blending scientific insights with a deep understanding of your individual circumstances. Together, you can develop a strategy that aligns with your goals, ensuring that each decision is made with care and maximizing your chances of IVF success.
Dr. Lucky Sekhon
My name is Lucky Sekhon and I'm a double board-certified OBGYN, and Reproductive Endocrinologist & Infertility specialist practicing at RMA of New York. My mission is to empower women with practical and scientifically accurate information to make the right fertility decisions for themselves.
Follow me on Instagram to keep up to date with my fertility related posts and content.

